About 30 to 85% of patients with musculoskeletal pain suffer from Myofascial Pain Syndrome. It usually manifests in the population between 27 to 50 years old and, when in its chronic aspect, this pathology is related to the occurrence of musculoskeletal pains that last 6 months or more.
What is myofascial pain syndrome?
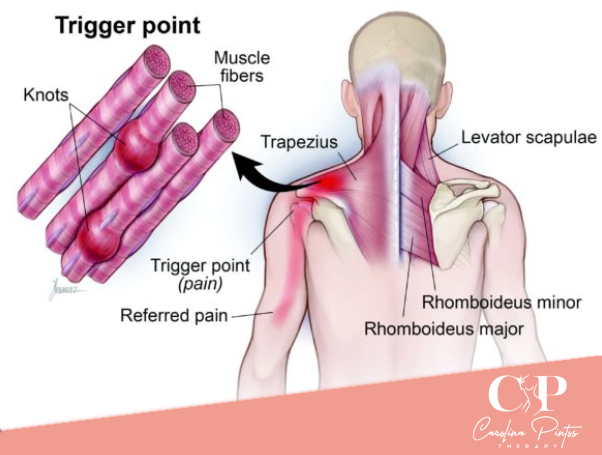
Myofascial syndrome is a condition of acute or chronic pain characterized by pains originating in the muscle and surrounding fascia. Patients with myofascial syndrome usually either have pains in restricted areas, or referred pains, which are painful sensations caused in regions that are not related to the physiological point originating the pain. For example, a headache that, in fact, has as a reference of origin a condition in the cervical musculature. Usually, patients are not aware that a pain is referred until a “Trigger Point” is stimulated and causes a painful sensation.
Among the most common signs and symptoms of myofascial pain syndrome, we have: recognition of pain on palpation of a “Trigger Point”, specific pain reference pattern, and rapid muscle contraction response to needling or palpation.
What is myofascial release?
Myofascial release is a physiotherapy technique that consists of pressing specific points of the body in order to release the fascia, which is a fibrous tissue that covers the muscle tissues.
The occurrence of muscle pains is associated with inflammatory processes that can affect the myofascial layer, which makes the fascia more contracted, narrow, and adhered to the muscle layer.
What are trigger points, and how do they influence referred pain?
Trigger Points are hyperirritable nodules, which are found along a tense band within a skeletal muscle and can be readily identified by palpation by trained therapists. These points were identified by light microscopy techniques, which showed contraction knots and narrowing of the endomysium (layer of connective tissue composed of reticular fibers that surrounds the muscle tissue) of the muscle fibers.
Trigger Points are classified as active or latent. Active Trigger Points are found in symptomatic patients, while latent ones are found in patients without pain. However, even latent Trigger Points have the ability to reduce the functionality of the muscles, making them mechanically inefficient.
How does myofascial release improve the prognosis of myofascial syndrome?
According to the systematic review by Desai, Mehul J et al. (2013), manual therapies, such as the myofascial release technique, constitute the most effective non-pharmacological treatment methods for the treatment of Myofascial Pain Syndrome by inactivation of Trigger Points.
The action of myofascial release massage consists in restoring the structure and texture of the fascia as the movements are applied. With this, the contracted knots of the fascia fibers return to their original state and deactivate the Trigger Points causing the referred pains.
Conclusion
In a randomized and placebo-controlled study, published in 2017 in the journal “American Journal of Physical Medicine & Rehabilitation”, with the title “Responsiveness of Myofascial Trigger Points to Single and Multiple Trigger Point Release Massages. A Randomized, Placebo Controlled Trial”. The efficacy of myofascial release treatments for increasing the pain threshold at trigger points in people with myofascial syndrome manifesting as tension-type headache was analyzed.
In this study, 62 individuals with tension-type headache were analyzed, who were randomized to receive 12 massages twice a week, for 45 minutes. The massages were focused on releasing the Trigger Points in the bilateral upper trapezius and suboccipital muscles. The pressure threshold for pain was measured with a pressure algometer before and after the first and at the end of the 12th treatment.
As a result, it was obtained that the pressure threshold for pain was increased at the trigger points, a fact that denotes a proof of the efficacy of myofascial release for the reduction of pains associated with Myofascial Pain Syndrome.
Sources
- Tantanatip A, Chang KV. Myofascial Pain Syndrome. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499882/
- Capó-Juan MA. Cervical myofascial pain syndrome. Narrative review of physiotherapeutic treatment. An Sist Sanit Navar. 2015 Jan-Apr;38(1):105-15. Spanish. doi: 10.23938/ASSN.0058. PMID: 25963463.
- Desai, Mehul J et al. “Myofascial pain syndrome: a treatment review.” Pain and therapy vol. 2,1 (2013): 21-36. doi:10.1007/s40122-013-0006-y Moraska AF, Schmie
This writing is the original and exclusive property of Carolina Pintos and is protected under copyright law. Unauthorized use of the same without the express consent of Carolina Pintos will be subject to prosecution under applicable laws.